Duchenne muscular dystrophy
Duchenne muscular dystrophy (DMD) is a type of muscular dystrophy that causes weakness and a wasting of the muscle due to low levels of a protein called dystrophin. If the body is lacking dystrophin, muscle cells become damaged and movements such as getting up from the floor and walking become a problem.1
In DMD, muscle weakness worsens as time goes on and daily tasks become harder. Eventually, the muscles in control of the lungs and heart will also stop working, although this usually takes several years.2,3
Everyone is different and so the DMD symptoms each individual experiences will differ in terms of progression and severity. However, most will experience some of the stages shown in the figure.2–6
What is Duchenne muscular dystrophy?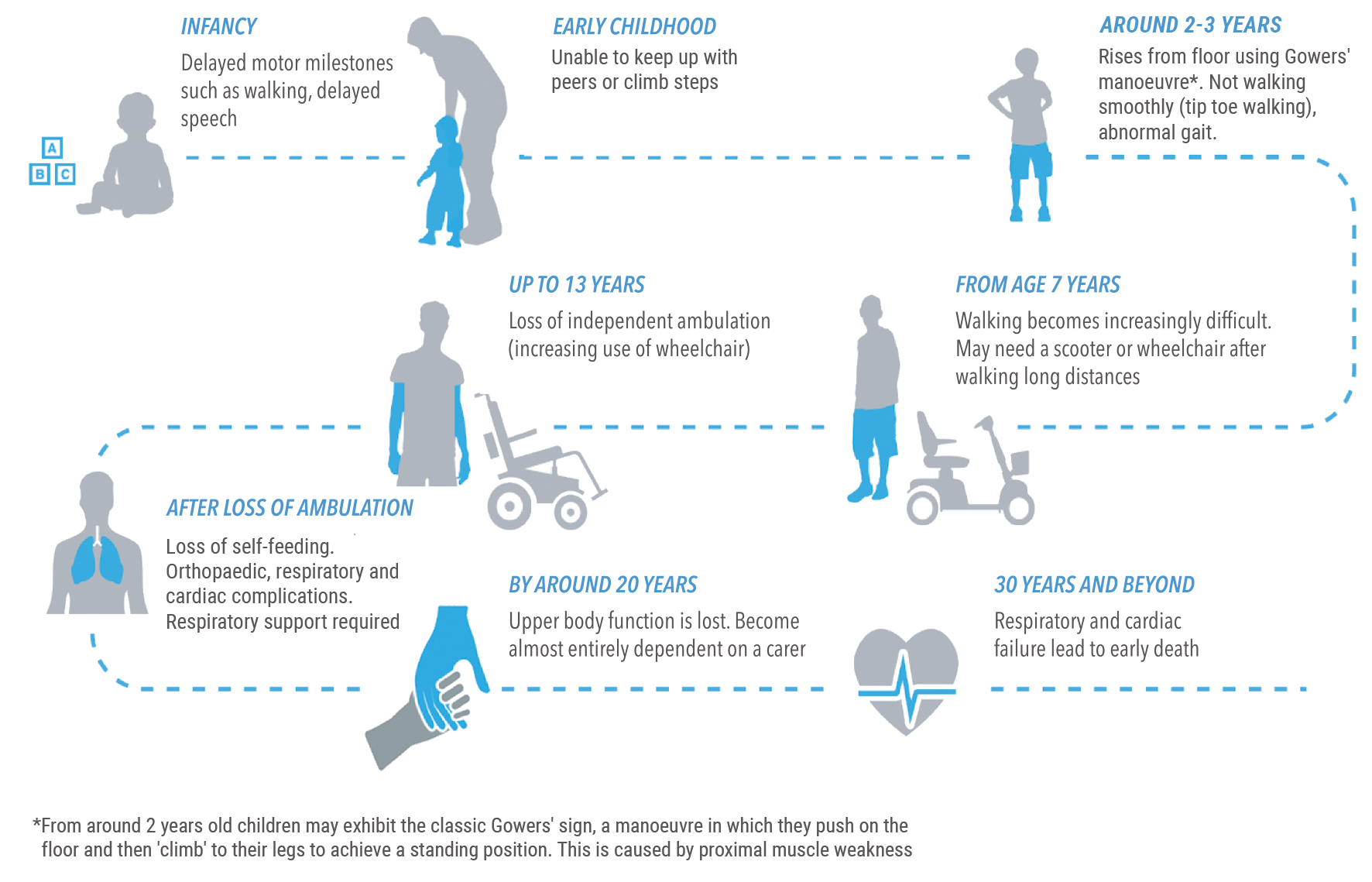
DMD causes
DMD is caused by the body not producing enough dystrophin, a protein that acts as a shock absorber for muscles.2,3,7
In DMD, the lack of dystrophin is caused by a gene change (mutation) that prevents the body from manufacturing enough of this important protein.2,3,8
How lack of dystrophin leads to the symptoms of DMD
When there’s a lack of dystrophin in the body, muscle cells become sensitive to damage, susceptible to injury and, over time, the muscles deteriorate.7
The body then replaces the injured muscle with fat and scar tissue, which impacts the ability of the muscle to function.7,9
The lack of dystrophin and the subsequent deterioration of muscle are what leads to the symptoms of DMD.2,3
Find out more about Duchenne muscular dystrophy’s causes and inheritance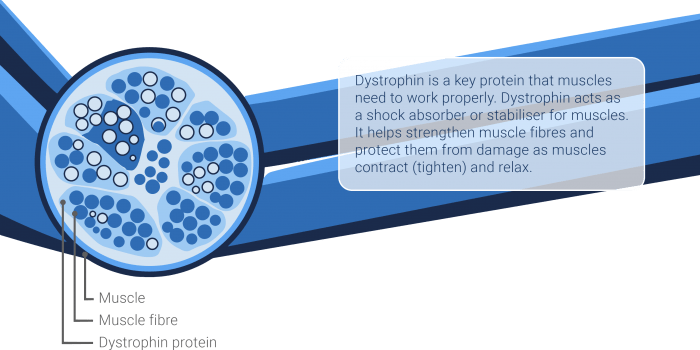
The genetic cause of DMD
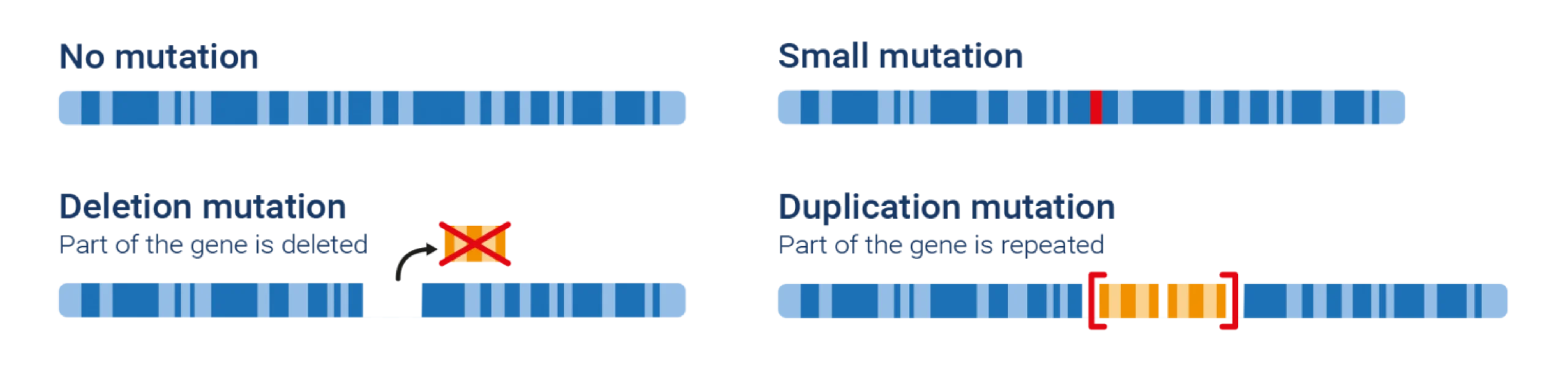
Mutations, or genetic changes in the gene that codes for the dystrophin protein, are the underlying cause of DMD.2,3
Genes are essentially the instruction manual for protein production. Proteins create and replace cells in the body.
In DMD, a mutation occurs in the gene that contains the instructions for making dystrophin – a key protein that helps to keep muscles functioning correctly.10 As a result, the body cannot make enough dystrophin for normally functioning muscles. Without the dystrophin protein, muscle cells can become damaged easily.3,9
What kind of genetic disorder is DMD?
DMD can be caused by various kinds of mutations. Large deletions in the dystrophin gene are the cause of most cases of DMD. But, sometimes DMD-causing mutations can be due to repetition or duplications within the gene, disrupting the code so that the body cannot read the instructions for producing dystrophin. Smaller changes in the DNA code can also cause DMD.9,11
Characterising the type of genetic mutation is required to optimise a patient’s treatment regimen, as some DMD treatments only target specific mutations.11
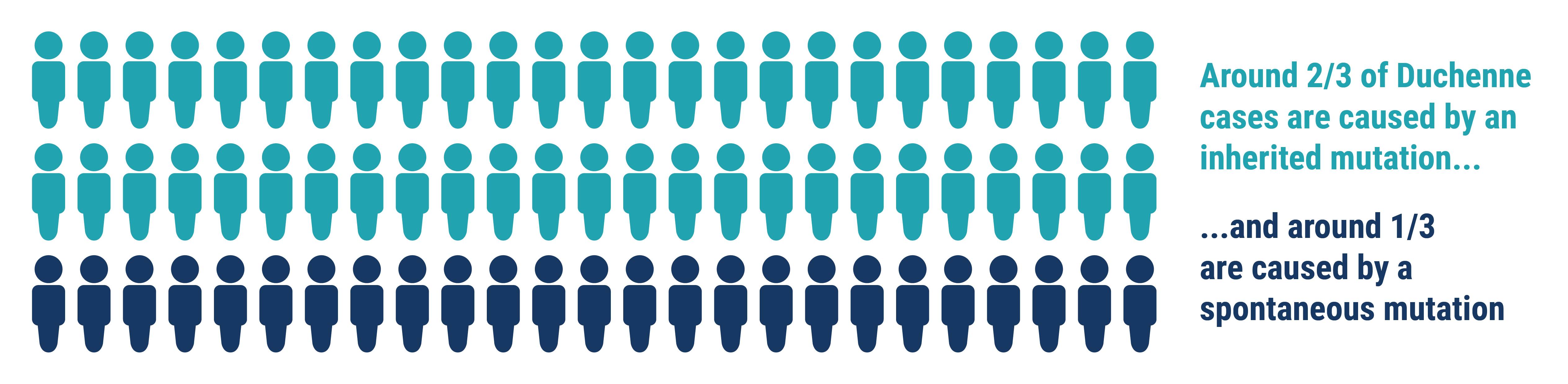
How do the genetic mutations that cause DMD happen?
The mutation in the gene that codes for dystrophin can either be:12,13
- Passed down through the family (inherited), or
- Caused by a new genetic change – this is called a ‘spontaneous mutation’
While spontaneous mutations occur without any family history, these new mutations can be passed down to children.12,13
The dystrophin gene is the largest known human gene, so it is more at risk of spontaneous mutations than smaller genes.2
New mutations can occur in an egg cell in two ways:
- The mutation occurs when the mother’s body makes the egg cell:13 If this egg cell is fertilised, the baby will carry a faulty dystrophin gene
- The mutation occurs at conception (when the mother becomes pregnant):14 In this case, the baby will carry a faulty dystrophin gene
When the baby grows up, they can pass the faulty dystrophin gene on to the next generation.12,13
Want to find out more about how Duchenne muscular dystrophy is caused?
Read more about Duchenne muscular dystrophy's inheritance and causesHow is DMD inherited?
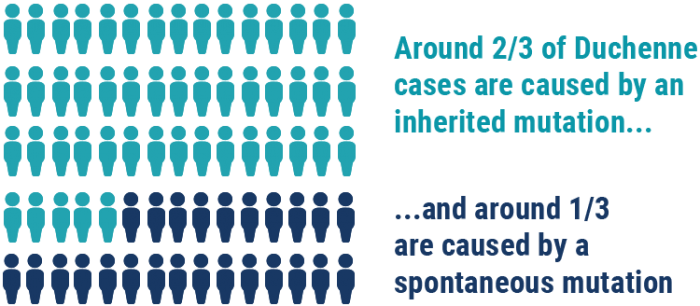
The gene that causes DMD is located on the X chromosome. DMD is therefore known as an X-linked disease.3
Boys inherit one X chromosome from their mother and a Y chromosome from their father. A boy will have DMD if his X chromosome contains a faulty dystrophin gene.13
Girls inherit an X chromosome from each parent. If one of their X chromosomes contains a faulty dystrophin gene, they still have a ‘back-up’ copy of the dystrophin gene, which normally compensates for the faulty one. A girl with a faulty dystrophin gene is called a ‘carrier’.13
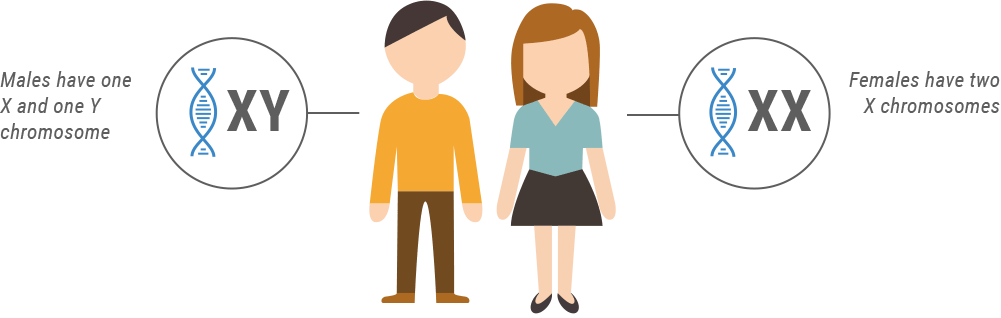
*Carriers may show signs and symptoms of DMD and may need treatment
Interested in learning more about how Duchenne muscular dystrophy is inherited? Click the link below.
Find out more about Duchenne muscular dystrophy inheritanceCarriers of DMD
Duchenne muscular dystrophy (DMD) is X-linked. An X-linked disorder is one in which the gene causing the disease can be found on the X chromosome.3 As girls have two X chromosomes and boys only have one, almost all affected individuals with DMD are male, while females are carriers. A genetic carrier is someone who has inherited the faulty gene that causes a certain disorder but does not necessarily show symptoms.13
Normally, DMD carriers do not show symptoms because if a girl inherits the faulty dystrophin gene, she has a healthy ‘back-up’ copy of the dystrophin gene on her other X chromosome. This usually compensates for the faulty one and produces enough of the dystrophin protein.13
However, sometimes a carrier is unable to produce enough dystrophin so will experience some signs and symptoms of DMD. This can be treated in the same way as boys with the condition.13
DMD may affect future pregnancies
The chances of a carrier having a child with DMD are 1 in 4 (or 25%). This means that for every baby she has, there is a 1 in 4 chance that the child will have DMD.13
It is important that all carriers have regular check-ups for strength, and to monitor their hearts, in order to ensure that any potential symptoms are treated correctly.13 It is vital for female relatives of a child with Duchenne muscular dystrophy to undergo testing in order to discover whether they are a carrier of the condition.
Read more about how Duchenne muscular dystrophy is inherited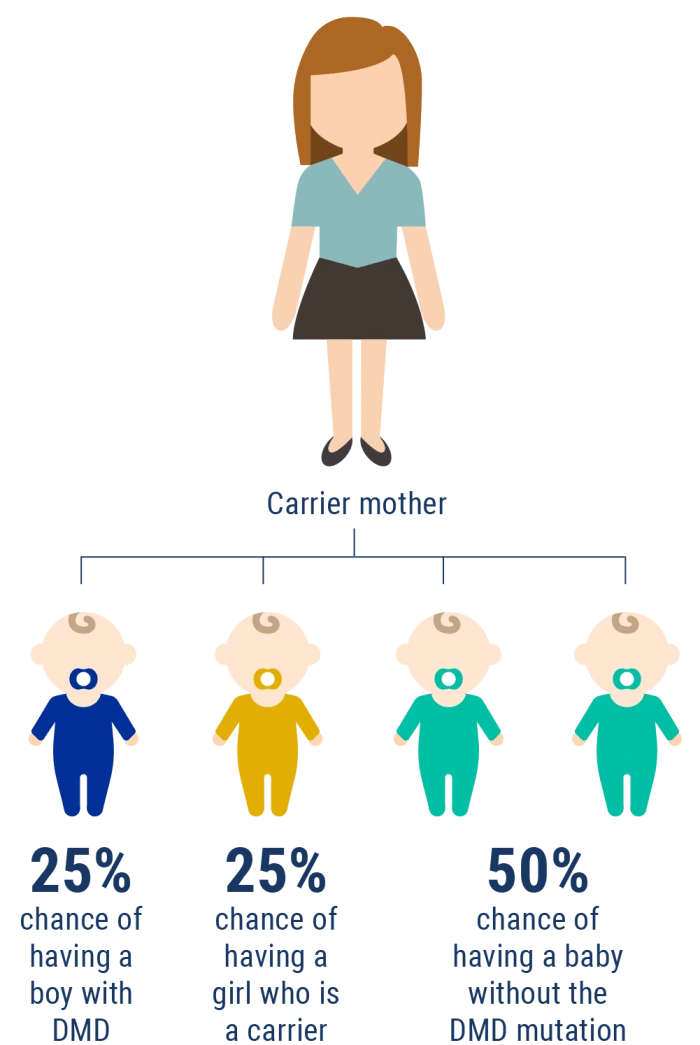
DMD signs and symptoms
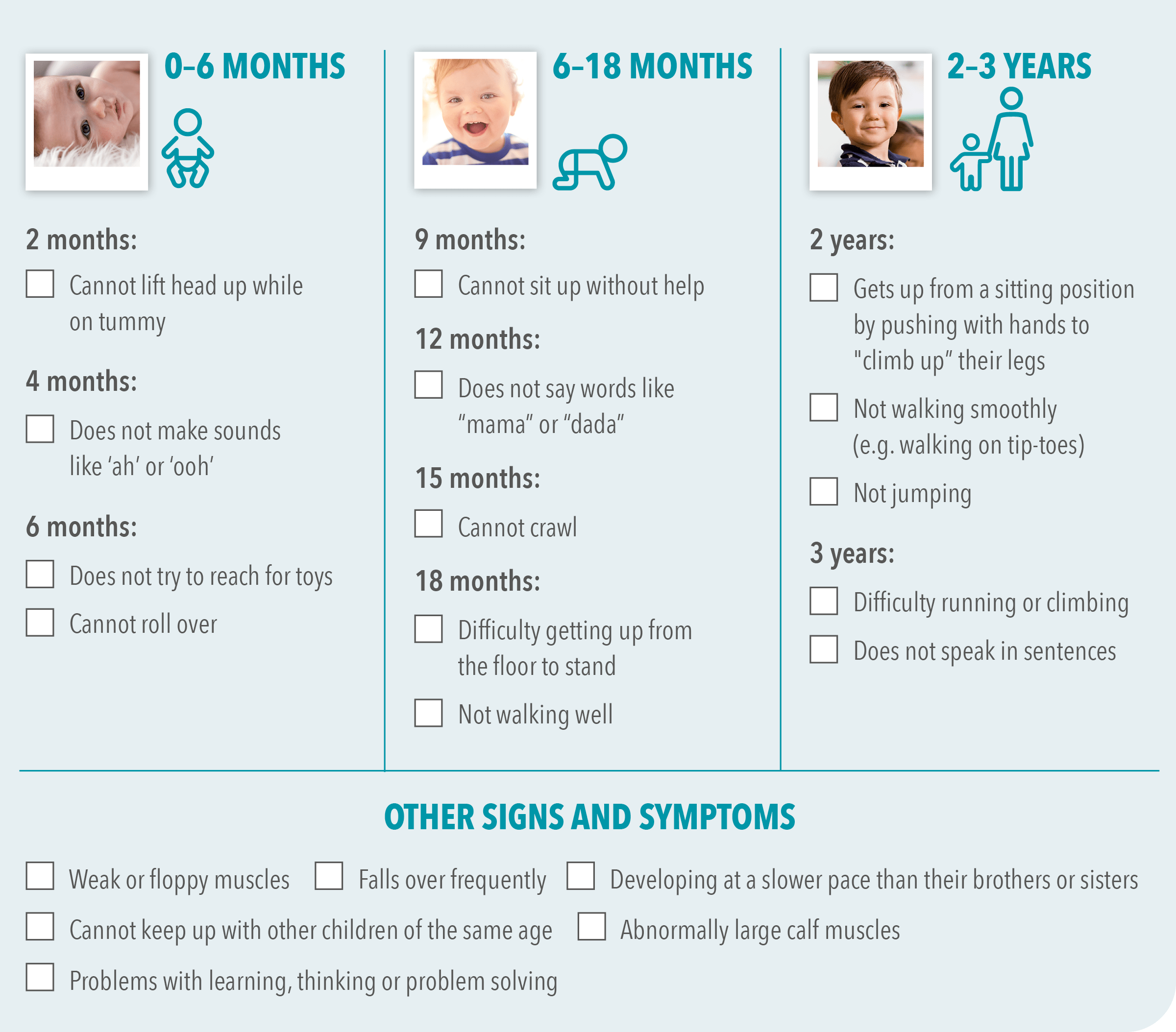
Most often a child not reaching developmental milestones when expected is the first noticeable sign of DMD. Developmental milestones include things like lifting their head, sitting, walking and talking.
Often, a delay in development is nothing to worry about. Every child develops differently, and there is a wide range of what is considered to be ‘normal’. However, in the rare situation that there is a problem, finding it early can ensure your child gets the help they need to reach their full potential.3,5,15
When to suspect DMD
Signs of a muscle problem include if your child is not walking well by 18 months, or cannot get up from the floor to stand.3,16,17
Other signs you may notice include:3,16–18
- Muscle weakness
- Delays in learning to speak
- Behavioural issues
- Tiring easily
- Developing slower than siblings
- Inability to keep up with children of the same age as them
There are many different symptoms of Duchenne muscular dystrophy. Click the link below to find out more
Learn more about the symptoms of Duchenne muscular dystrophySymptoms Q&A
By 2 months of age, most babies can usually lift their head while lying on their tummy. Not being able to lift their head could be a sign of a muscle problem. Read more about this symptom of DMD.
Most babies begin to make ooh and ah sounds by the age of 4 months. If your baby has not started to babble or make happy noises, it could be a sign of developmental delay. Read about speech delay and DMD.
Most babies start trying to roll over when they are about 6 months of age. If your baby is older than 6 months and not rolling over, it could be time to talk to someone about developmental milestones. Find out about developmental delay and DMD.
By 9 months, your baby should be able to sit up unaided. If they still need your help or the support of cushion and pillows, it may be a sign of a muscle weakness. Read more on muscle weakness in DMD.
Healthy children should be able to climb the stairs independently by age 2. If your child is struggling with this activity after age 2, it could be a sign of developmental delay. Find out more about this DMD symptom.
There are many signs and symptoms that can indicate your child may have a muscle weakness. Children all develop differently, and what is considered to be ‘normal’ can vary greatly between individuals. Discover more about DMD symptoms.
By the age of 3, most children will begin to talk in sentences. Every child develops their talking skills at different speeds, and what is ‘normal’ can look and sound very different depending on many factors. Find out more about this sign of DMD.
Walking on tip toes can be a sign of a muscle problem. Discover more about DMD symptoms.
Every child develops differently. Not hitting specific milestones could be a sign of developmental delay, but it’s worth remembering that there is a wide range of what is defined as ‘normal’. Find out about milestones and DMD.
If your baby has low muscle tone, they can feel very limp when you hold them in your arms – this is often referred to as ‘floppy baby syndrome’ and can be a sign of muscle weakness. Read about more DMD symptoms.
Do any of these FAQs apply to your child?
Find out more about the signs and symptoms of Duchenne muscular dystrophyThe signs of DMD in everyday life
It’s not always easy to recognise some of the more common signs of DMD. Symptoms that indicate developmental delay, such as walking with an unusual gait and not being able to keep up physically with other children of a similar age can be easy to overlook.
To see what these symptoms might look like in everyday life, and to understand the importance of spotting them as early as possible, watch this animated video.
Find out more about the symptoms of Duchenne muscular dystrophyDevelopmental milestones checklist
As a parent or caregiver, it’s very useful to become aware of milestones and what your child or young person is accomplishing.
We have created a useful developmental milestone checklist to help you keep track.
The checklist below has been designed to help you understand:
- What your child or young person should be able to do according to his or her age
- The warning signs that could indicate a developmental delay
DMD diagnosis

If your doctor suspects DMD, they will first undertake a physical examination for muscle weakness. Your doctor will also ask about delays in early developmental milestones, such as sitting, walking and standing up.

Your doctor will normally recommend a type of blood test called a creatine kinase (CK) test if your child or young person shows signs and symptoms of DMD. This involves taking a small blood sample to send to a lab for analysis.

If your doctor decided that further testing is required, they will normally refer them to a specialised centre or neuromuscular specialist. Doctors who specialise in DMD will then undertake a careful diagnostic process to uncover what has been causing the symptoms. As part of this, they might suggest a number of tests.

If high CK levels are detected, an additional blood sample may be taken to test for genetic changes (mutations) that cause DMD. These genetic tests might verify the diagnosis of DMD, or exclude DMD as a possibility.
If DMD is confirmed:
There are therapies and resources available to support you in managing the symptoms and potentially slow down disease progression.
If DMD is excluded:
Your doctor will undertake further enquiries in order to find out the cause of the symptoms your child is experiencing. A variety of genetic tests can be used to inform your doctor of the kind of mutation your child has. Different therapies and resources are used to provide support for different mutations, so these additional tests are vital.

A CK test checks for an enzyme called creatine kinase, or CK. When muscle fibres are damaged, CK leaks out into the bloodstream. The muscle damage caused by DMD means that the level of CK in the blood will often be higher than normal.3,18 High CK levels in the blood do not automatically mean that your child or young person has DMD. Genetic testing is the only way to confirm a DMD diagnosis.

Once your child has been diagnosed, they can start to receive the specialty care and treatment they need for DMD.3
Prenatal testing for DMD
During pregnancy prenatal tests can be carried out to discover whether the growing baby will be affected by DMD.3,19
This information is important because:
- If the baby has DMD, you can choose if you would like to continue the pregnancy19
- Achieving an early diagnosis of DMD has been demonstrated to enhance outcomes for patients and enable families to access the support and care that they need earlier3
Are you eligible?
You may be eligible for prenatal diagnoses in future pregnancies If you have a child or relative with DMD.19 After you’ve received the results, you can discuss what these mean for your family with your genetic counsellor. To find out more about prenatal testing and whether or not you are eligible, speak to your doctor.
Learn more about the process of diagnosing Duchenne muscular dystrophy
Read more about the diagnosis of Duchenne muscular dystrophyWhy early diagnosis is important
If your child or young person has DMD, it is better to find out sooner rather than later.3,18 This will allow them to receive medical care for their condition sooner. The earlier they are able to begin their treatment, the greater opportunity there is for slowing down the disorder and enabling them to maintain their muscle function for longer.3,18
With early diagnosis, the following benefits can be received sooner:
- Access to specialists3,18
- Early treatment initiation3
- Genetic counselling3,18
- The ability to apply for financial assistance*20–22
- The chance to register your child for clinical trials of new treatments3
- Access to support from patient organisations, and interactions with other families living with DMD21,23
- Family members at risk can be tested, and the potentiality of DMD in any future pregnancies can be discovered3,18
- You can begin organising your plans for caring for your child at home3,21
Luckily, there are treatment and management options that have a beneficial impact on the progression of DMD.24 Medications are available, as well as other treatments such as physiotherapy.
Medications can delay muscle function loss, which might help to slow the onset of difficulties in this area. This enables your child to remain mobile and live more independently for longer.3,25,26
Three ways appropriate management can help: 3,25,26

May slow the progression of the disease

May assist in symptom management

May enable your child to maintain their quality of life and independence for as long as possible
*Check with your local social care provider to find out what is available.
Early diagnosis is key to ensuring the best possible treatment for your child.
Find out what’s involved at the link below
Read more about Duchenne muscular dystrophy diagnosis
When you suspect something
is wrong
As a parent, you see how your child is developing every day. Feeling that something may be wrong – but not knowing what – can be stressful and frustrating.15,27
Take action now. Find out how Duchenne muscular dystrophy is diagnosed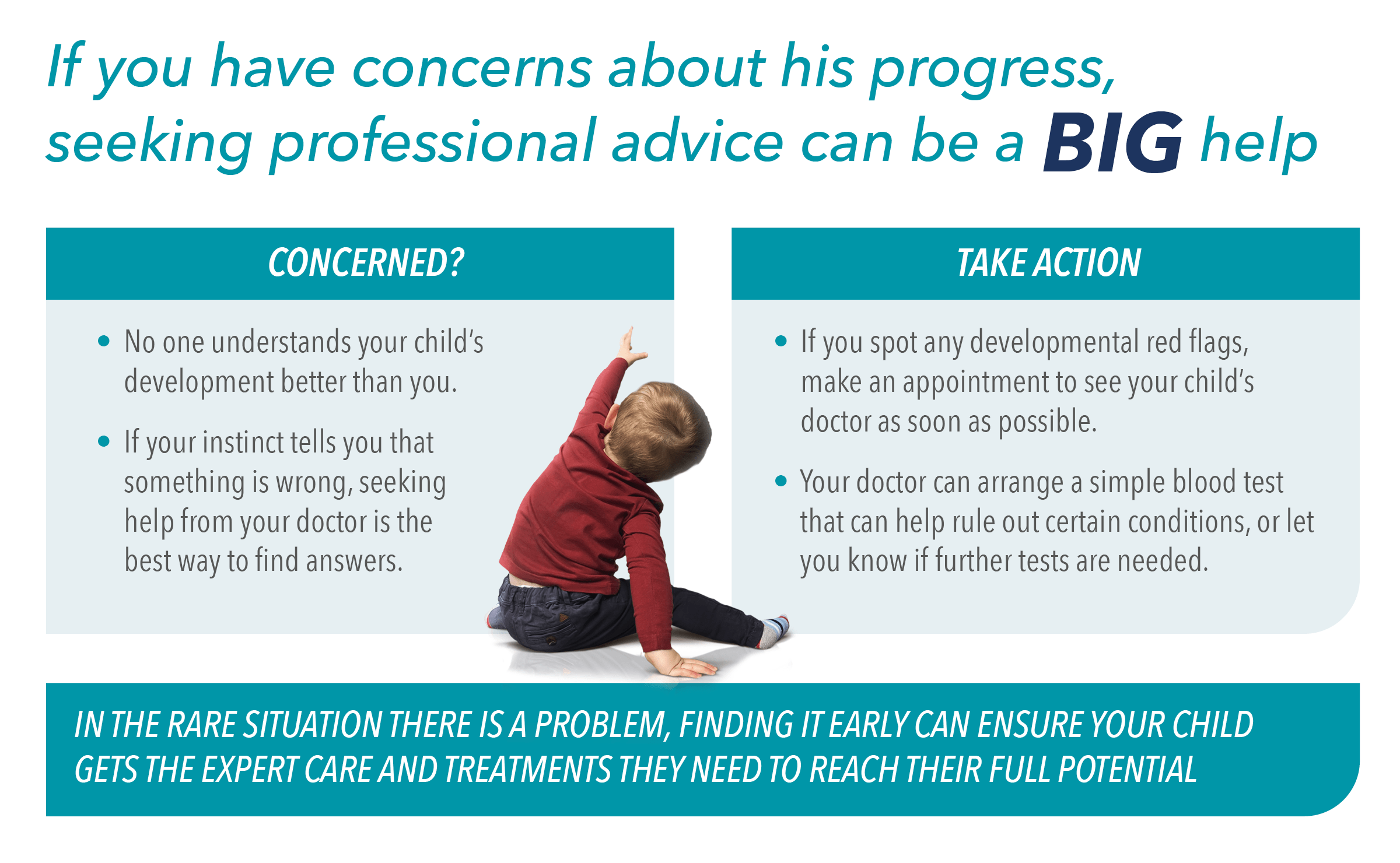
Genetic counselling for DMD
Genetic counsellors are professionals who can help guide you through genetic tests and explain the effect the results might have on your family. They are also able to support you emotionally and provide you with resources for long-term coping.
How can a genetic counsellor help me?28–30
A genetic counsellor will:
- Address your questions on Duchenne muscular dystrophy and its impact on your family
- Assist you in deciding upon the most effective testing strategy for your relative or child
- Enable you to understand the results of any testing, and decide upon a course of action
- Assist you and your family in coping with a positive test result
Talking to a family member about genetic testing
Deciding whether to talk to your family members about a genetic diagnosis is a very personal decision. But you are not alone.
A genetic counsellor can help you:
- Work out which family members could be affected by DMD28–30
- Understand the benefits and drawbacks of telling your family about DMD29,30
- Decide when and how to tell your family about DMD29,30
- Prepare what to say and decide what information you should share29,30
- Anticipate and prepare for any questions they might ask29,30
- Deal with any difficult emotions29,30
Interested in how a genetic counsellor can help you to navigate your Duchenne muscular dystrophy diagnosis?
Find out more about genetic counselling for Duchenne muscular dystrophyDMD treatments
DMD treatments fall under two key categories:
- Medications: which slow down the loss of muscle function and assist in symptom treatment.3,31
- Supportive care: which enhances a patient’s quality of life and helps them to deal with the difficulties of DMD. Physiotherapy, breathing support, and heart monitoring all fall under supportive care.3,31
Options for DMD medications
Medications are available that can ease symptoms and protect muscles. The varying symptoms of DMD can be treated with specific medications:3,6,25,31
Drugs to reduce muscle cell inflammation3,6,25,31
These drugs help DMD patients to maintain muscle strength for longer. They might also enable patients to maintain their lung and heart strength for longer and delay the onset of scoliosis. They are the most frequently used medications for DMD.
Drugs to assist muscle cells in creating dystrophin25
DMD is caused by a mutation in the gene that codes for dystrophin. Dystrophin is a protein that enables muscles to function correctly. In a patient with DMD, dystrophin cannot be produced.
These drugs target the cause of the condition and help the body to create a working form of dystrophin.
The medications currently available for this purpose are only appropriate for some DMD patients, because of the way that they function. For this reason, it’s important that your child undergoes genetic testing as soon as possible, in order to find out the specific mutation causing their DMD. This will enable your care team to decide upon the correct management pathway.
Possible new treatment options are emerging, a few of which are in the clinical trial stage. Your child’s doctor will be able to advise you on treatment options.
Medications for the heart31
DMD patients are susceptive to developing a heart condition called cardiomyopathy. This condition cuts down the heart’s capability to pump blood, resulting in potential eventual heart failure. This condition can be treated with a variety of medications.
Medications for the bones31
DMD patients frequently have weak bones and might develop osteoporosis, which increases bone fragility. Muscle weakness and particular drugs can contribute to the development of osteoporosis in DMD patients. It is possible for bone strength to be improved.3,25,31 Speak to your doctor for further information.
Vaccinations3,6,25,31
To assist in preventing infections, DMD patients might be offered the flu (influenza) and pneumonia (pneumococcal) vaccines.
There are a variety of treatments for Duchenne muscular dystrophy
Find out more about treatments for Duchenne muscular dystrophyWorking with your care team
Finding out that your child has DMD can be hard, but your care team are here to support you and provide you with help and information when you need it.
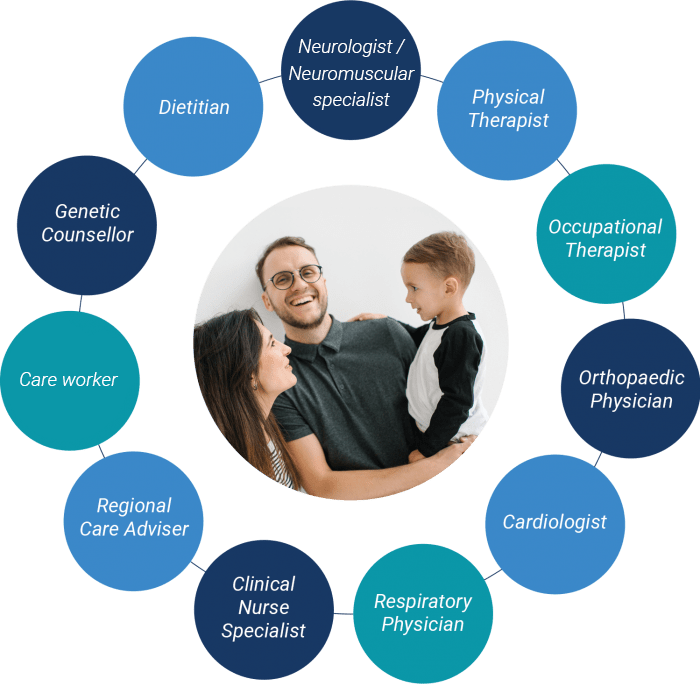
Your Duchenne muscular dystrophy team might comprise of:
Neurologist3,32
A specialist in disorders of the brain, nerves and spinal cord. This specialist frequently organises the rest of the care team.
Orthopaedic physician3,32
A healthcare professional whose focus is on disorders of the bones and joints.
Cardiologist3,32
A healthcare professional whose focus is on disorders within blood vessels and the heart.
Respiratory physician3,32
A healthcare professional whose focus is on lung diseases.
Physical therapist3,32,33
A healthcare specialist who helps patients to enhance the working of their muscles and joints.
Occupational therapist3,32,33
A healthcare specialist who assists children in learning the abilities they need to participate in everyday activities.
Clinical nurse specialist31
A nurse whose focus is on working with Duchenne muscular dystrophy patients.
Social worker / psychologist / psychiatrist3,32,33
Someone who assists patients and families in adapting to the diagnosis of Duchenne muscular dystrophy and helps them to contact any necessary services. This professional may also contact a child’s school to ensure that they have the correct systems and equipment to adequately support the child’s needs.
Dietitian3
A health specialist focused on nutritional therapy, who can provide therapy and guidance to patients with DMD.
Regional care advisor3,31
Someone who supports patients and families with Duchenne muscular dystrophy from a practical, emotional, psychological and social perspective. They also advise families on finding equipment and services.
Genetic counsellor3
A healthcare specialist whose focus is on medical genetics and providing genetic counselling.
Interested in finding out more about the way in which Duchenne muscular dystrophy is treated?
Find out more about Duchenne muscular dystrophy treatmentWhat to expect with DMD
The symptoms of DMD are different for each child, and the rate at which symptoms worsen varies.3,5 As time goes on, the symptoms of DMD will change:34
- As the muscles get weaker, the ability to walk is slowly lost3,34
- As the back muscles become weaker, the spine may begin to curve (called scoliosis)34
- In late childhood to early adulthood, the upper body and arm muscles also weaken34
- The heart and respiratory (or breathing) muscles also weaken over time, which can lead to complications3,34
As DMD is a progressive disease, meaning the symptoms become more apparent over time,3,9,34 it is important to get your child the right treatments and management as soon as possible.3,5 This gives your child the best chance of maintaining their independence and quality of life for as long as possible.3,5,33
Duchenne muscular dystrophy can impact every aspect of your family’s life.
Ensure you access the support you need

What are neuromuscular disorders?
Find out more about the family of diseases known as neuromuscular disorders

What is Duchenne muscular dystrophy?
Find out more about the most common type of muscular dystrophy

Duchenne muscular dystrophy causes and inheritance
Learn how Duchenne muscular dystrophy is passed down through families

Duchenne muscular dystrophy symptoms
Understand the key signs and symptoms of Duchenne muscular dystrophy
References
- National Institute of Neurological Disorders and Stroke. Muscular dystrophy: hope through research. Available at https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Hope-Through-Research/Muscular-Dystrophy-Hope-Through-Research [last accessed March 2021]
- Goemans N, et al. Eur Neurol Rev. 2014;9:78–82.
- Birnkrant DJ, et al. Lancet Neurol. 2018;17:251–267 [Part 1].
- Noritz GH, et al. Pediatrics. 2013;131:e2016–e2027.
- van Ruiten HJA, et al. Arch Dis Child. 2014;99:1074–1077.
- Bushby K, et al. Lancet Neurol. 2010;9:77–93.
- Houang EM, et al. Skelet Muscle. 2018;8:31.
- Muscular Dystrophy Association. Duchenne muscular dystrophy (DMD). Available at https://www.mda.org/disease/duchenne-muscular-dystrophy/research [last accessed March 2021].
- Amato AA, Brown RH Jr. Muscular dystrophies and other muscle diseases. In: Longo DL, et al., editors. Harrison’s principles of internal medicine. 19th edition.
- Ervasti JM. Biochim Biophys Acta. 2007;1772:108–117.
- Kalman L, et al. J Mol Diagn. 2011;13:167–174.
- Duchenne UK. What are the causes of DMD? Available at https://www.duchenneuk.org/faqs/what-causes-duchenne [last accessed September 2022].
- Muscular Dystrophy Association. Causes/inheritance. Available at https://www.mda.org/disease/duchenne-muscular-dystrophy/causes-inheritance [last accessed September 2022].
- National Institutes of Health. What is a gene mutation and how do mutations occur? Available at https://ghr.nlm.nih.gov/primer/mutationsanddisorders/genemutation [last accessed September 2022].
- Lurio JG, et al. Am Fam Physician. 2015;91:38–44.
- World Health Organization. Six gross motor milestones. Available at https://www.who.int/childgrowth/standards/mm_windows_table.pdf [last accessed September 2022].
- National Task Force for Early Identification of Childhood Neuromuscular Disorders. Guide for primary care providers. Available at https://childmuscleweakness.org/wp-content/uploads/2019/05/PrimaryCareProviderPacket.pdf [last accessed September 2022].
- Aartsma-Rus A, et al. J Pediatr. 2019;204:305–313.e14.
- Bianco B, et al. Einstein (Sao Paulo). 2017;15:489–491.
- Muscular Dystrophy News. Assistance fund opens program to help Duchenne patients with medical expenses. Available at https://musculardystrophynews.com/10/28/assistance-fund-offers-duchenne-muscular-dystrophy-patients-help-with-medical-expenses/ [last accessed September 2022].
- Parent Project Muscular Dystrophy. Funding sources. Available at https://www.parentprojectmd.org/care/for-families/community-resource-center/daily-life-resources/funding-sources/ [last accessed September 2022].
- Muscular Dystrophy UK. Financial and practical support. Available at https://www.musculardystrophyuk.org/get-support [last accessed September 2022].
- World Duchenne Organization. Mission & vision. Available at https://www.worldduchenne.org/mission-vision/ [last accessed September 2022].
- Muscular Dystrophy Association. What is…Duchenne muscular dystrophy. Available at https://www.mda.org/sites/default/files/2019/03/Duchenne_Muscular_Dystrophy_Fact_Sheet.pdf [last accessed September 2022].
- Mah JK. Neuropsychiatr Dis Treat. 2016;12:1795–1807.
- Gloss D, et al. Neurology. 2016;86:465–472.
- Cyrus A, et al. PLoS Curr. 2012;4:e4f99c5654147a.
- Helderman-van den Enden ATJM, et al. Clin Genet. 2011;79:236–242.
- Institute of Medicine (US) Committee on Assessing Genetic Risks; Andrews LB, et al., editors. Assessing genetic risks: implications for health and social policy. Washington, DC: National Academies Press (US); 1994: 4. Issues in genetic counseling. Available at https://www.ncbi.nlm.nih.gov/books/NBK236049/ [last accessed September 2022].
- Parent Project Muscular Dystrophy. Genetic counseling. Available at https://www.parentprojectmd.org/about-duchenne/is-it-duchenne/genetic-counseling/ [last accessed September 2022].
- Birnkrant DJ, et al. Lancet Neurol. 2018;17:347–361 [Part 2].
- Muscular Dystrophy UK. Care advisors and clinical nurse specialists. Available at https://www.musculardystrophyuk.org/get-support [last accessed September 2022].
- Birnkrant DJ, et al. Lancet Neurol. 2018;17:445–455 [Part 3].
- Sussman M. J Am Acad Orthop Surg. 2002;10:138–151.
© 2022 PTC Therapeutics.
GL-DMD-0669 | October 2022